ON Nov 9, Pfizer announced the interim results for its Covid-19 vaccine candidate: more than 90 per cent effective. A week later, Moderna reported its vaccine’s late-stage trial results of 95pc efficacy, followed by Russia’s Sputnik vaccine at over 92pc efficacy. Not to be left behind, the interim results for the Oxford vaccine showed an overall efficacy of 70pc, which rose to 90pc when the dosages were adjusted.
Together, these candidate vaccines have opened up the prospect of turning the tide on the deadly Covid-19 pandemic. Yet they also come attached with associated issues of affordability, accessibility and coverage — all of significant concern for low- and middle-income countries. With rich nations already cornering a major chunk of vaccine production lines, widely voiced fears of inequity in distribution have now acquired a sense of urgency.
Both the Moderna and Pfizer vaccines are expensively priced and require considerable cold chain capacity, trained staff and quick readiness for complex vaccine deployment arrangements. The Oxford vaccine, meanwhile, is cheaper, easily transportable and storable at normal temperatures. On these grounds, it is being hailed as the most suitable vaccine for low- and middle-income countries.
However, the Oxford vaccine is set to go through further trials due to its mixed efficacy results before it gets to the emergency authorisation stage, while the Pfizer and Moderna ones are likely to be waved through by the US Food and Drug Administration by the second week of December. With these dates in mind, the US and Europe are ramping up vaccine delivery and deployment mechanisms. The UK has already appointed a full-time minister to oversee the roll-out, signifying how seriously vaccine deployment is being taken by the government.
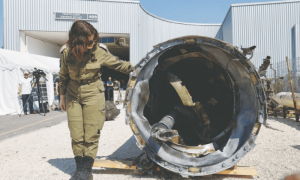
As vaccines are rolled out, affordability and access will be major issues.
Pfizer has already concluded purchase agreements for 100 million doses with the US government, 40m doses with the UK and 120m doses with Japan. The EU will buy up to another 300m doses. This pre-ordered and pre-purchased vaccine production is set to generate a supply deficit for developing nations where the need is high due to underpowered and under-resourced health systems. After supplying pre-orders, less than a quarter of production is left for the rest of the world.
To offset this inequity, the World Health Organisation has launched the COVAX initiative, which aims to deliver two billion doses to developing nations by the end of 2021. This projected supply will go some way towards ensuring equitable access. Despite this lofty declaration, however, Pfizer has yet to sign a purchase agreement with COVAX.
Last month, the Indian and South African governments asked the World Trade Organisation to not give countries the power to either grant or enforce patents linked to Covid-19 drugs and vaccines until global immunity is achieved, with UN human rights experts backing this call.
Yet this call has gone nowhere. According to current projections, Africa is not likely to get a vaccine before mid-2021. Some countries have already placed orders for new vaccines, including India and Nepal in our region. Pakistan will also get vaccine supply through COVAX and other global mechanisms. Yet this will take some time to kick in.
Whether Pakistan’s grossly under-reported case numbers will be a factor in the allocation of vaccines is not yet clear. But setting aside $150m for advance purchase is a step in the right direction. Given the less than ideal response during the first wave, the government must ensure that advance purchase of appropriate vaccines is made to at least initially cover healthcare workers.
Against the backdrop of limited supply, priority groups are already being identified worldwide. These include healthcare workers, the elderly and people with pre-existing conditions. In the UK, a joint committee on immunisation will decide the priority groups. Alongside these developments, all countries are pressing ahead with speedy vaccine roll-out plans.
Vaccine deployment policies in Pakistan should be devised by a high-level advisory committee composed of public health experts, infectious disease specialists and virologists. It would inadvisable to see a repeat of the case of unequal distribution of personal protective equipment, which reportedly ended up with the non-healthcare elite first and the deserving healthcare staff second during the first wave of the pandemic. A well-coordinated and well-considered roll-out is what is urgently needed to ensure priority groups are vaccinated in the first round, followed by equal access to a Covid-19 vaccine for all.
The writer is a public health consultant and author of Patient Pakistan: Reforming and Fixing Healthcare for All in the 21st Century.
Twitter: @arifazad5
Published in Dawn, December 9th, 2020