What are Covid-19 anti-bodies? Does it help to test for them? Here's what is known so far
As Covid-19 ravages through the population, the latest buzz word around town is immunity and the bounties that it promises. There is talk of "immunity passports" which, based on antibody tests, will enable the positive ones to re-join society, keeping the negative ones sequestered for the safety of all. Attractive as this may sound, there are several scientific and ethical reasons why this concept is problematic for society.
Let us first examine the science behind antibody testing.
Immunity: Execute, control, and conclude
The first line of defence against infection are the cells that are on surveillance duty in the body, the White Blood Cells. They recognise common patterns on invading pathogens, the viruses or bacteria, and mop them up as best they can. However, if the invaders start to infiltrate cells and multiply, or the initial assault is overwhelming, the body triggers a specific immune response and this is where the much acclaimed antibodies start being produced.
These antibodies help by preventing the virus from entering and infecting new cells, or coating the virus so that it is then easily targeted by surveillance cells and destroyed; the final victory resulting in a sea of antibodies. In addition to orchestrating the initial victory, they also create a reservoir of memory cells, so that a subsequent attack by the same offender will be dealt with promptly and efficiently. Therein lies the promise of the antibody response.
Antibody response to Covid-19, as we know it
From what we know so far, following infection by the virus Sars-Cov2 that causes Covid-19, detectable IgM and IgG antibodies develop within days to weeks from the onset of symptoms in infected individuals, but are detectable in only about 20% of patients during the early part of the disease. However, by the 3rd or 4th week since the symptoms' onset, almost all patients develop IgM and IgG, with a simultaneous increase in both.

Five weeks after the onset of symptoms, the IgM begins to decline, almost disappearing by week 7. IgG however remains persistently elevated beyond the seven week period. Why some patients do not seem to develop detectable antibodies and an immune response is still uncertain.
With regards to this particular virus, there is still uncertainty regarding the relationship between antibody response and clinical improvement. The findings from a small study of nine patients with Covid-19 found that greater clinical severity produced higher antibody titres. However, antibody detection and higher titres have not always been found to correlate with clinical improvement in Covid-19.
The long-term persistence and duration of protection conferred, if any, by antibodies currently remains unknown for this disease. Even though anecdotal reports have appeared about reinfections, there is no clinical data to indicate whether these are actual new events with the same virus or a relapse of a smouldering infection. As is obvious, there are still a lot of ambiguities around the Covid-19 related antibodies to start celebrating them as guarantors of our freedom.
Antibody based research in Pakistan so far
Sensitivity of the test is heavily dependent on the prevalence of the infection in the population. With no accurate population based estimations yet, we have some preliminary prevalence data of Covid-19 in our population from a recent report published in the daily Dawn by Getz Pharma which carried out antibody testing on 2,174 asymptomatic individuals working in the company’s head office in Karachi.
They used a test reportedly with high sensitivity (the ability to correctly detect positive cases) and specificity (the ability to correctly detect negative cases) for both IgG and IgM.
While the total positive cases they found were 8.6%, when stratified into different groups, the seroprevalence in high-risk frontline hospital workers was 11% and seroprevalence in families of positives contacts was 19%. All these numbers indicate is that those tested had been exposed to Sars-Cov-2 virus and while they did not show any symptoms themselves, they had developed an antibody response.
Depending on where you carry out your study, you could get different prevalence because of the population that has been included in the study. New York, the first state in the US to do its own antibody testing, found an estimated 13.9% prevalence rate. The rate was even higher in New York City, at 21.2%. when they sampled 3,000 people who were out shopping. Whereas, another study from a county in Los Angeles showed about 2.8% to 5.6% of their adult population having antibodies.
In order for the test to be used on the entire population, it must be technically validated to ensure that performance is reliable, reproducible, and accurate. If the test seems to be able to distinguish those with disease from those without, and if the test results seem to be sufficiently robust, its clinical validity and accuracy then needs to be cross checked by matching results of PCR testing from actual patients who are confirmed as having the disease. From research published so far, we do not have any evidence that antibody detection or titre (quantity) correlates with clinical status of Covid-19, including infectivity and protective immunity.
The Getz study results, though of academic interest, are not generalisable since they did not perform a population-based study. Furthermore, the seroprevalence does not indicate whether these individuals were themselves infective since there was no simultaneous viral RNA testing (PCR) performed.
What does the antibody test tell us at this point?
A positive antibody test tells us that the individual was infected by the virus in the past. As indicated above, the rise and fall of IgM and IgG antibodies follow a specific pattern and if tested within these windows, there is a high likelihood of them being detected. Having said that, an infection with a poor viral load may not elicit a detectable antibody response; similarly people with compromised immunity may also not mount a response and may test negative even when they have had the infection.
A positive test does not indicate a current ongoing infection, or that the individual is carrying the virus. Also, a positive test does not mean that the individual is now definitely clear of the virus and should be considered safe, posing no threat for spreading infection, since in some cases, the virus and infectivity from it may still be there even with a detectable antibody response.
This means that contrary to what is being advocated regarding antibody tests being useful in reopening the public space to positive individuals, it must be cautioned that a person with antibodies may still be a potential spreader. A positive test also does not indicate that the individual is safe from getting a Covid-19 infection again, since we do not know the nature, extent, or duration of any immunity that the antibodies confer. Much depends upon the quantification of the antibody titres and their correlation with future events, a point where we have not yet scientifically arrived.
With further scientific progress, of course, we may actually be able to glean this information with these blood tests. At this point, the accuracy of a test says little about whether patients who undergo the evaluated test(s) are better off than similar patients who have not been tested, or who have been tested with a different test. The presence of multiple tests for determining antibodies, each claiming superiority over the other, compounds the confusion.

Unlike other viral infections like Hepatitis B and C for instance, where antibody tests are the mainstay of evaluation, this is not the case yet for the virus causing Covid-19, and the clinical utility of measuring antibodies for this new virus is as yet not clear. Given what we know at the moment, the greatest utility of antibody tests for Covid-19 infections is in helping in determining a more accurate prevalence and case fatality rate across the population. So far, we have only been able to estimate the prevalence and fatality rate by using total number of detected cases as a denominator through the cumbersome and expensive PCR testing on nasopharyngeal swabs. This limits the numbers of those who can be tested. The measuring of antibodies in blood is faster and cheaper and can therefore be used for screening large populations. The federal government is reportedly planning on conducting a seroprevalence study across the country, after initially piloting in Islamabad using antibody tests, along with PCR.
Regulations governing use of antibody tests
Despite a wave of manufacturers promoting the test globally, including rapid tests with reports available in minutes, there are serious reliability concerns. Global regulatory bodies have also been voicing concerns and have produced recommendations on how and when the test may be used.
The FDA itself does not endorse or validate antibody testing for diagnosis of Covid-19 infection. Their website states that "based on the underlying scientific principles of antibody tests, the FDA does not expect that an antibody test can be shown to definitively diagnose or exclude Sars-Cov-2 infection".
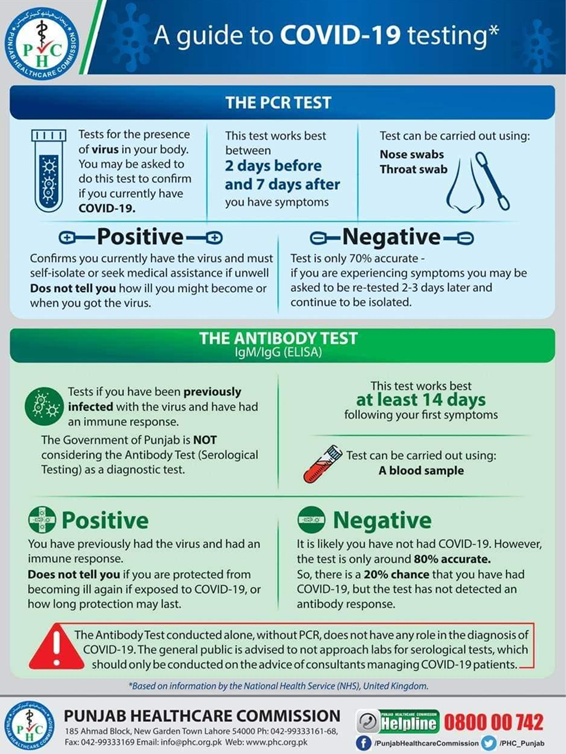
Closer to home, the Punjab Healthcare Commission, after initially banning antibody tests in Punjab has now permitted them under strict guidelines.
Immunity license or certificates
This brings us back to the debate about "immunity passports". As described above, we are not at a point scientifically to determine immunity or otherwise against Covid-19, which is why this cannot be deployed at the moment. But it will perhaps be a matter of time when we actually do come up with a convincing and accurate test denoting immunity.
However, even if the science is sorted out, there are ethical grounds on which this kind of "licencing" concept can be problematic.
Access to tests will be limited to begin with, depending upon availability and affordability. This means that the better connected and the affluent would have an unfair advantage of getting tested and obtaining the back to a normal life "passport" sooner than the poorer citizens. This will further augment the marginalisation of underprivileged.
In addition to further stratification in an already fragmented society, this will lead to increased resentment because of the potential of discrimination.
Moreover, stigma has been a major fallout of this pandemic for Pakistanis and this kind of certification, or the lack of it, is bound to enhance that problem and add to the adverse psychological impact due to it. In a country where it is far easier to get a fake driver’s license than take an official driving test, getting an immunity certificate will be a piece of cake.
The desperation for obtaining this license may lead to reckless behaviour on part of a public which already demonstrates a lack of compliance to safety SOPs. People may be tempted to expose themselves to the virus in order to mount the coveted antibody response which they hope would ultimately lead them back to jobs and livelihood. A positive result might evoke a false sense of security and promote less adherence to precautions. Furthermore, if the false positive rate is 5%, then five out every 100 individuals would think they are 'protected' when that actually may not be the case and could in fact lead to disease spread.
In time, we will discover what it really means to have antibodies to Covid-19, and what it means to not have them. The focus should be on using our knowledge of them to promote health, and not as another means of compartmentalising our fragmented society into yet another category of haves and have-nots.
Header photo by Shazia Hasan