The Covid-19 emergency and prioritising public health in Pakistan
Little more than three months ago, no one knew Covid-19 existed. And yet, as the first quarter of 2020 draws to a close, the virus has spread to nearly every country on the planet, infecting over 800,000 people and claiming tens of thousands of lives. Economies are tanking, overloaded healthcare systems are crumbling, and general panic is gripping populations as the modern life that we know has been disrupted to an end that most people have never imagined, yet alone witnessed.
The rapid onset of Coronavirus, and its mushroom growth around the world has caught governments and the public by surprise. And yet the inevitability of a global pandemic has been on the radar for years. In 2015, following a global outbreak of the Ebola virus, Microsoft Co-Founder Bill Gates discussed at length preparedness for what he called "The Next Outbreak" in a TED talk that has now been viewed more than 23 million times. The key takeaway was the establishment and enhancement of proactive public health systems, particularly in developing countries.
Organised efforts to improve the health and well-being of communities are as old as humanity itself; indeed, the origins of historical medical interventions can be traced back thousands of years through historic and religious texts.
Over the years, the concept of "public health" has evolved to include not only implementing health goals, but to also build on social values to shape proactive systems that have the capacity to cope with disease outbreaks and pandemics. The boundaries of public health have blurred, with new health and social issues combined with a political, economic, and ideological shift.
Also read: Pakistan's dilapidated health system bent double with COVID-19 scare
Thus the domain of public health focuses on the entire spectrum of health and well-being, not only the eradication of particular diseases. The history of public health has been one of identifying health problems, developing knowledge and expertise, and rallying political and social support around solutions. Although health needs and health services have not diminished, political and social values of current times encourage fiscal constraint. Consequently, the goal of public health is now linked with scientific analysis of disease, medical treatment of individuals, and education on healthy habits.
Institutional and systematic health inequalities continue to persist in developing countries like Pakistan. This is in part due to preventive health programmes lacking a focus on the broader economic, environmental, and underlying socio-cultural factors impacting health and health services delivery. Furthermore, rapid globalisation and urbanisation, combined with demographic and nutritional challenges compound an already ominous situation. The challenges don't end there; for skilled workforce shortages, inefficient distribution of resources, and the ever present threat of epidemics and pandemics combine to create a treacherous uphill battle.
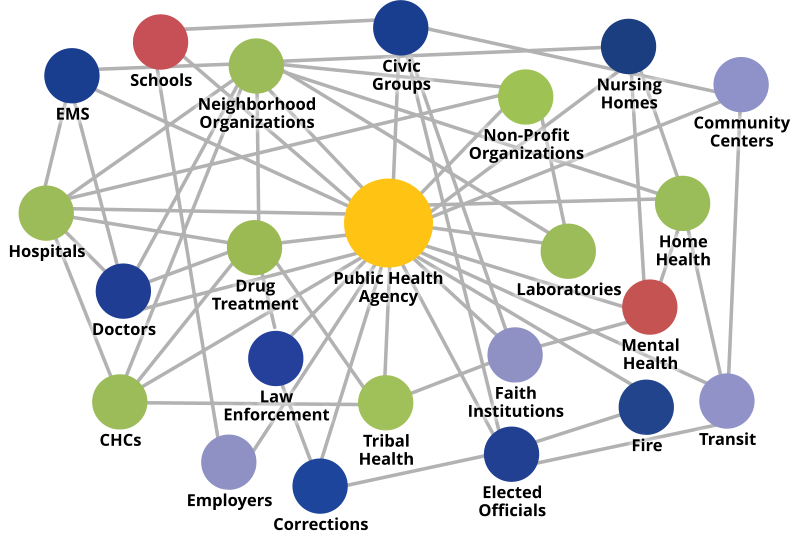
Research shows that cross-cutting factors which influence individual and collective health do not work in isolation. There is a pressing need to understand the dynamic relationships between these actors and their impact. The coronavirus outbreak is one such example, that has transcended boundaries and sectors. From a global economy that has now been declared in recession to prioritising production of ventilators under the Defence Production Act, Covid-19 has emerged as a formidable foe to governance and public health systems around the world.
Pakistan’s current sector-specific approach with little acknowledgement, coordination, and recognition of interlinked stakeholders and factors does little to help in crises like these. Public health in particular, has seemingly been at the bottom of the priority list; whether the challenge is long term like smog; medium term like dengue, or more immediate and severe like heat waves and droughts. The cherry on top is the deep mistrust among the public and private sectors; the latter often being looked at as competitors and negative disruptors rather than as valuable partners.
More on this: With Covid-19, healthcare workers are having to choose who gets a chance to live, and who will be left to die
The Global Health Security Index, which assesses countries in terms of pandemic preparedness, places Pakistan at the 105th position out of 195 countries. The ranking drops considerably in terms of healthcare infrastructure, communications during public health emergencies, infection control, and availability of equipment.
Public health functions are rigidly fragmented, with limited resources, expertise, and powers vested under dozens of ministries, authorities, and institutes. The lack of an overarching institutionalised mechanism for coordination, real-time monitoring, predictive modelling, policy formulation, legislation, and workforce planning and development continue to lead to disastrous outcomes.
The International Association of National Public Health Institutes (IANPHI) highlights several key public health functions, defined after years of research and understanding best practices from its 100 member countries. This includes disease surveillance, investigation of pandemics and epidemics, promotion of relevant research, and evidence based policy making in partnership with public and private stakeholders in the health sector. These recommendations are based on one core underlying assumption; that there is no single model for a national public health institute. Rather it is left up to the decision makers to decide the major public health issues affecting a particular country; and nurturing a setup that shares core attributes and functions with the international standard.

The US Centers for Disease Control and Prevention (CDC) recommends a public health system based on combined efforts by healthcare providers, public safety agencies, social and charitable networks, education and youth organisations, and environmental agencies. Some of the essential public health interventions proposed by the CDC include community level interventions, such as educating people about health issues, effective local monitoring, and harnessing community level action to tackle health challenges. Additionally, legislation and policies to support health promotion, linking people to personal health services, assuring provision of care, and developing a competent workforce are also required. Finally, the accessibility, effectiveness, and quality of health services needs to be constantly re-evaluted in light of research and innovation.
In 2017, Punjab government embarked on a short-lived project to establish "Punjab Public Health Agency"; which was envisioned to promote public health in the province through effective health surveillance and reporting; analysis and investigation of threats to public health; and policy formulation. PPHA was planned out as a vital component of the province's Integrated Disease Surveillance and Response (IDSR) strategy by offering technical and scientific expertise in order to tackle the challenge of infectious diseases.
Read further: Humans of pandemic
The agency also planned to house a Data Repository Unit to serve as the information hub for all health data in collaboration with the Punjab Information Technology Board (PITB). Additionally, commissioning and facilitating research in all avenues of health, workforce planning, strategising and policy formulation, communication, and coordination across departments, provinces, and ministries were also entrusted to the agency. This effort to bring fragmented expertise, knowledge, practice, and skill under one roof would have been a highly effective solution in terms of preparedness, resilience, and response to health emergencies.
The SARS-CoV-2 pandemic is a reminder of just how well-prepared we are — at a governmental, institutional and public level — to tackle public health emergencies. Such emergencies are further compounded by looming workforce shortages in the health sector. For example, Pakistan is well on its way to become the most nurse-short country in the world. Experts estimate that nearly a million nurses will be required in Pakistan in the next few years — and the annual rate of adding to the nursing workforce is less than 10,000. Similarly, there are no dedicated epidemiologists in the Disaster Management Authorities; whose critical services could have reshaped our response to the Covid-19 pandemic.
The need of the hour is to lay down the foundation for a multi-sectoral organisation that is able to lend its expertise for policy formation and structural reforms in healthcare and allied sectors. Ensuring cross-sectoral participation necessitates the engagement of a broad group of stakeholders. In addition to tackling existing and future health challenges, predictive modelling and artificial intelligence to identify future areas of intervention, and meeting the targets of the Sustainable Development Goals, the underlying focus should be on improving the quality of public health around the country.
It is also imperative for leading educational institutes in the country to prioritise health education with an emphasis on management. One such initiative has been undertaken by LUMS; which will train the next generation of practitioners in the areas of healthcare policy, innovation and entrepreneurship in healthcare, and managing healthcare operations.
The health impact pyramid, a framework for public health action, postulates that addressing socioeconomic factors has the greatest potential to improve individual and community health. This does not imply that other interventions should be ignored; different solutions may be more cost-effective and feasible in different situations. What holds true however, is that interventions to preserve and promote the health of the public need not only the support of government and society, but dedicated political will and sustainable funding in order to succeed. Pakistan’s healthcare system has performed well when these elements have come together; for example, the country was the first in the world to eradicate Guinea-worm disease. Similarly, the lady health visitor/worker programme has also been lauded for its efficacy. The time to act is today, before our already overloaded healthcare system begins to crumble.